Benefits Guide | 2026
VDHP/Traditional PPO with Ortho
Option 1 – New Medical Plan: Value-Driven Health Plan (VDHP)
About The VDHP Medical Plan
The VDHP Medical Plan is designed to give you more control, more transparency about costs upfront, and often more savings. This plan uses Medicare pricing (plus a negotiated percentage) to establish fair rates for medical services, creating a solution that’s mutually beneficial for you and your providers. In many cases, members enjoy lower out-of-pocket costs and greater flexibility when choosing where to receive care.
The VDHP Medical Plan is a copay plan. There are no deductibles so that you are aware of any associated costs up front.
There are also no network restrictions. The VDHP Medical Plan provides open access to hospitals, both inpatient and outpatient facilities, physicians and ancillary providers (such as labs and therapists) with no network restrictions. As a result, there’s no worry or concern about going to a provider that is “in-network.”
Dental insurance coverage is included with the VDHP Medical Plan.
How The VDHP Medical Plan Works
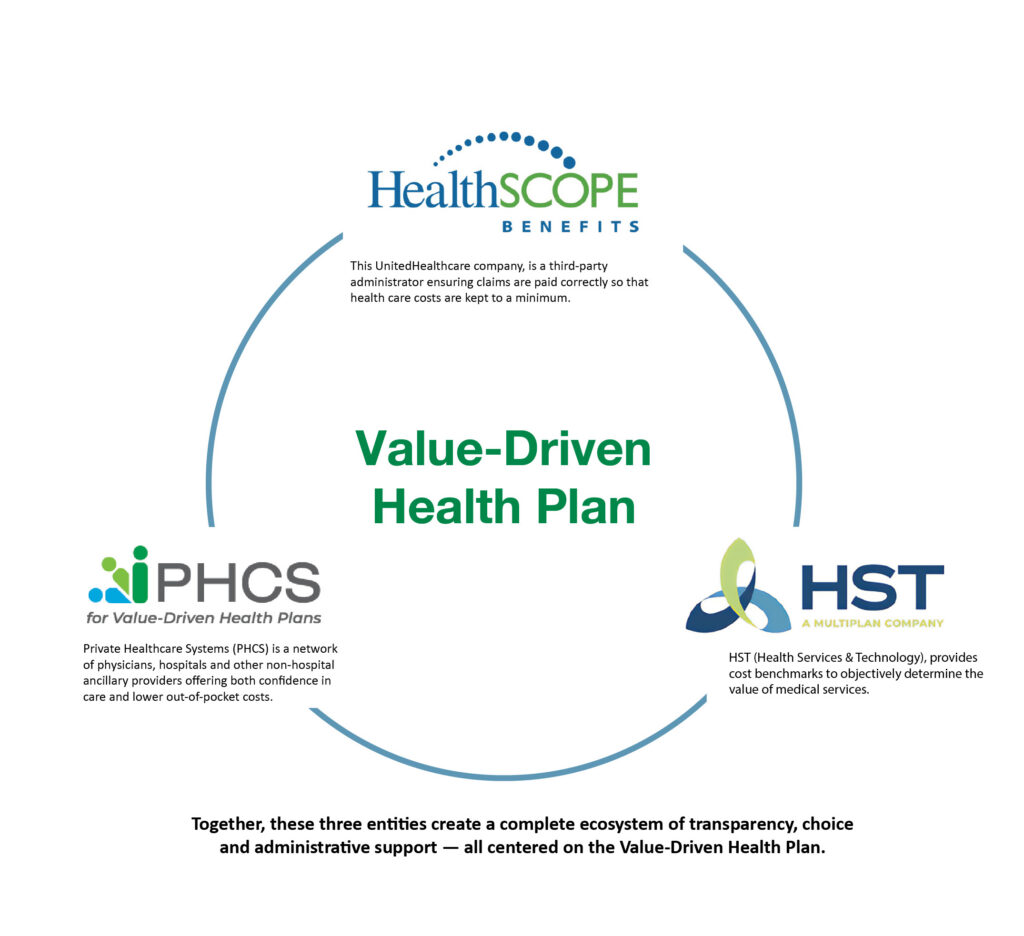
The Value-Driven Health Plan works by bringing together three key components. Each plays a unique role in delivering transparent, flexible, and supportive health care services.

About the VDHP Medical Plan
The following video provides key highlights that explain how the VDHP Medical Plan helps you get the most from your healthcare benefits.
About Pathways Concierge Services
Learn about how Pathways Concierge Services provides support to guide you through your benefits and assist you with any questions or items specific to your health care needs.
Patient Advocacy Center (PAC)
If you receive an unexpected bill from a provider, PAC educates, communicates and negotiates on your behalf with them. They are your advocate, contacting the provider and ensuring you are billed fairly and accurately. If you wish to choose a provider with a low acceptance rate of the negotiated pricing or that is out of the PHCS network, PAC can help you understand the risks and potentially help negotiate with the provider before your medical service.
VDHP Medical Plan Frequently Asked Questions
How do I search for a provider?
You can search for providers on the following link: HST-PHCS Provider Search
You can also use the HSTConnect mobile app for access to quality, cost effective health care in the palm of your hand. The HSTConnect mobile app features include:
- Search for a provider in the PHCS network with high acceptance rates
- Direct dial providers and get driving directions
- Access to HST’s Provider Acceptance Rates
- Compare quality ratings and pricing for specific procedures
- Prescription pricing estimates
- Submit balance bills directly to PAC through the app
- View copays and receive notifications
- Look up information about procedure
- Communicate and receive notifications from Patient Advocacy Center (PAC)
How does HST price claims?
HST’s pricing methodology uses Medicare (plus a percentage) to determine a fair and reasonable price for medical services.
How do I know how much I will be charged for my procedure?
By utilizing HSTConnect you can view your estimated cost up front. You will be responsible for your copay up to the annual out-of-pocket max.
Will my current providers accept VDHP Medical Plan insurance? What if they don’t?
Since the VDHP Medical Plan is based on fair and transparent pricing, most providers will work with your plan and file claims on your behalf. However, as with any plan, providers may need more information. If the doctor is not familiar with VDHPs or the PHCS network, you can instruct the doctor to call the provider number listed on your Medical Benefit ID card. If the doctor is in the PHCS network, you will be seen. The Pathways Concierge Service can also help you navigate issues that may arise and will work directly with your doctor on any specific questions they may have.
What happens if a provider balance bills me?
If a provider bills you for an amount above the patient responsibility identified on your Explanation of Benefits (EOB), don’t just pay the bill! Instead, contact the Patient Advocacy Center and a Patient Advocate will work with you, take over your case and deal directly with the provider so you don’t have to. They will stay in touch with you throughout the process until the claim is resolved.
Enroll by Oct. 31 Open
Do you have questions?
Feel free to call our Benefit Specialists to assist you with any questions or issues you have with the enrollment process.
(800) 941-7089
